
Hospital Bag Checklist
8 min read | 9 September 2019
8 min read | 20 February 2022

Listen to Season 3, Episode 5 above or on Apple Podcasts or Spotify.
*Trigger warning: Please be aware that this episode contains content about infant loss and may be triggering to those who have experienced this.
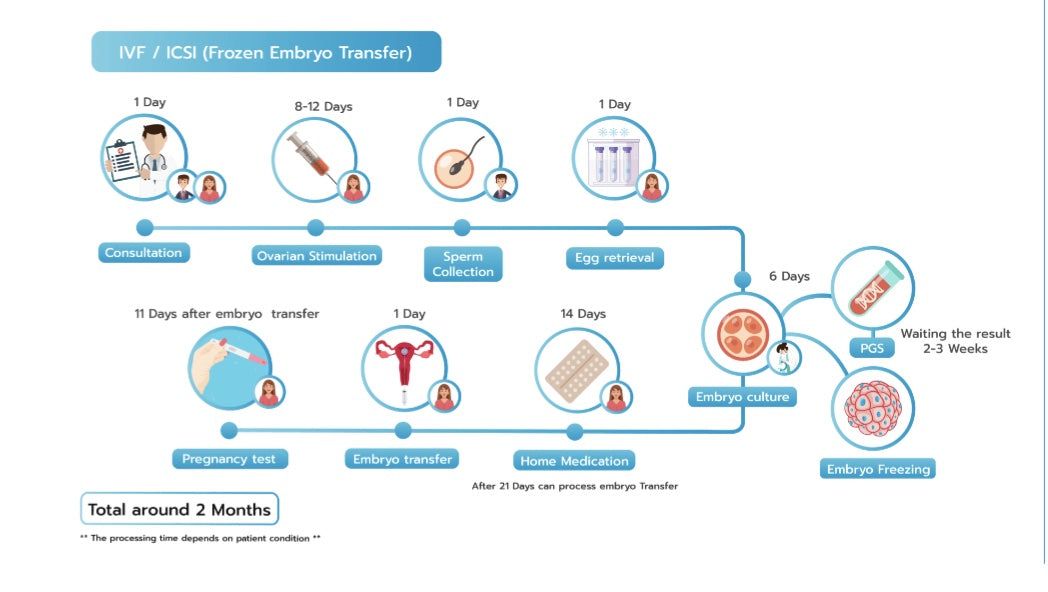
In-vitro Fertilisation (IVF) is a medical procedure where an egg is fertilised by sperm outside of the body. The process is undertaken in order to assist reproduction where there are issues of fertility of genetics.
People do not choose the path of IVF as their first option. Usually when someone turns to IVF, they have tried all other options to get a baby. There are a variety of reasons why people undergo IVF, including fertility issues, egg freezing due to age, life phase or illness. Others will also undertake IVF if they have the need to remove the possibility of a genetic condition or for same sex relationships that want a baby.
IVF can be different for each person. There are so many combinations for medications, timings, therapies, techniques – there is not a ‘one fits all’ process. It is also important to note that not everyone who sees a fertility specialist will end up doing IVF, there are a range of other options and stages depending on what the need for treatment is.
Generally, the process will begin when you start your period, you would then let your specialist know. They will tell you when to start taking a follicle stimulating hormone which aims to stimulate all of a woman’s follicles into producing an egg rather than just one which happens in a usual cycle. At a time determined by your specialist you will begin taking a second medication which stops your body from ovulating the eggs so that they can collect them.
When the majority of the follicles are measuring a size which indicates they likely have an egg inside them the specialist will tell you an exact time to take an injection called a trigger shot. This injection does the final maturation stage for the eggs. Egg retrieval occurs exactly 36 hours after the trigger injection.
Once the eggs are collected, they are put together with the sperm to fertilise. The embryos are watched closely for five to six days until they make a blastocyst. Not all eggs will fertilise and not all fertilised eggs will become blastocysts. It is a stressful and agonising wait.
Healthy blastocysts may be transferred straight away in what is called a fresh transfer; however, often embryos are frozen to be transferred later and can be tested for chromosome or genetic conditions.
*Image sourced from Genea.
Sadly, IVF is expensive and beyond reach for some people. Although there are public fertility clinics in Australia, many go through private IVF clinics due to wait times and success rates. The average IVF round will cost $6000 out of pocket after government subsidies. Not all IVF cycles cost the same as there are a variety of additional services that some patients need depending on their fertility issues that can increase the cost.
A round of IVFs success can be measured in a couple of ways. Mostly a successful round of IVF results in a healthy pregnancy and birth. However, there are a few other measures of success including developing and freezing healthy embryos for future use or identification of the reason for fertility.
IVF success rates really depend on the couple’s age and the clinic's methods and specialists. On average there is about a 40% success rate of a birth from an embryo that is transferred within a cycle. A woman aged between 35-39 years old has a 23% live birth rate from IVF.
Some aspects of IVF are covered by Medicare and private health insurance such as a portion of the medications or the day surgery for the egg collections.
A round of IVF including a fresh embryo transfer takes a month. However, for those who have a frozen transfer or need genetic testing it will take at least two months. In terms of the number of months it takes for success that can vary greatly. Some may only need one round/month whereas others may need several.
After IVF, if a woman is pregnant her care is transferred to her doctor, obstetrician or hospital. In most cases the pregnancy is treated like a pregnancy from a natural conception. If the IVF round is unsuccessful the patient will speak to their fertility specialist about the plan for the future which may include another round of IVF with changes to their protocol.
Tell people, don’t go through it alone.
Don’t be ashamed of going through IVF. Almost one in twenty babies are born through IVF.
Don’t automatically expect IVF to work. Many people need more than one cycle so it is important to be aware of that and be mentally prepared.
Prepare for IVF. An egg and a sperm have a 90 day lifespan so what you do for the three months before IVF can impact on the success.
Be kind to yourself through the process.
A genetic condition is a problem with health and/or development caused by faults in a person’s genes. Reproductive genetic carrier screening is a test that looks at an individual or a couple’s genetic information, to find out if they have an increased chance of having a child with a genetic condition.
It is recommended that genetic carrier testing is done before a person/couple begins trying for a baby to allow time for decisions to be made based on those results if deemed to be high risk. However, testing can be done up until the end of the first trimester in pregnancy.
Previously, only people with a family history of a genetic condition, or those in population groups where particular genetic conditions are more common, were offered reproductive genetic carrier screening. However, research now shows on average everyone carries approximately three to five genetic conditions, Therefore, it is now recommended that doctors offer information about reproductive genetic carrier screening to all prospective parents.
No, this is a different test. The non-invasive prenatal test (NIPT) look at the baby’s chromosomes to detect chromosomal conditions, such as Down syndrome. Chromosomal conditions are different to the genetic conditions screened for in reproductive genetic carrier screening.
This article was written by Rachael Casella (@mylifeof_love), in conjunction with Season three, episode 5 of Purebaby’s podcast, Pure Parenthood.
For more information on genetic carrier screening and Mackenzie’s mission. See here: https://www.mackenziesmission.org.au/
Sign up to Pure Love Rewards and get $10 off your first online order, earn points every time you shop and more!